PALLIATIVE CARE & HOSPICE CARE SERVICES
What Is Palliative Care?
Palliative Care is specialised medical care which is given to the patients suffering from any serious life limiting illness.
Aim Of Palliative Care?
It strives to improve the quality of life of patients and families affected by life-threatening ailments such as cancer, heart failure, chronic obstructive pulmonary disease, severe liver or kidney disease, alzheimer’s, parkinson’s disease, motor neuron diseases, neuropathies and many more.
Why Is Early Pain And Palliative Care Management Necessary?
Early palliative care improves the patient’s quality of life by relieving pain, controlling symptom burden, and providing psychological/spiritual/emotional support.
Main Causes Of Cancer Pain:
- Infiltration by tumour itself or compression over the nerves
- Metastasis to bone or joint space
- Peripheral neuropathy
- Degenerative changes in spine/joints – unrelated to cancer
How Is The Pain Management Done?
- Counselling in addition to pharmacotherapy by WHO analgesic ladder approach
- Minimally invasive pain and spine interventions (MIPSI)
- Implantable systems (Intrathecal / Epidural pump, SCS)
- Central desensitization therapy
Three Common Terms Used In Palliative Care To Understand:
Palliative care: It should begin as soon as a cancer or other chronic life-limiting illness is diagnosed. Palliative care is an approach that improves the quality of life of patients (including adults and children) and their families who are facing problems associated with a life-threatening illness. It prevents and relieves suffering through the early identification, correct assessment and treatment of pain and other problems, whether physical, psychosocial, or spiritual. It offers a care process that goes beyond the physical symptoms. It uses a team approach to address suffering and support the patients and their families, starting with the diagnosis, treatment phase, hospice care, end-of-life care, and providing bereavement counselling. Palliative care is explicitly recognized under the human right to health and is provided via a patient-centric approach. It is now an integral part of the health services system under global standards.
Hospice care: This term is used when the disease, such as advanced cancer, gets to a point when the treatment can no longer cure or control it. Hospice care denotes that the patient is expected to live approximately 6 months or less if illness runs the usual course. Goals of care here shift from cure towards care, control, and maintaining quality of life. When the cure to serious illness is not possible, or the patient chooses to not undergo disease directed treatments, it is time to label them as hospice care and counsel them to prepare for the next phase of life i.e, end of life care.
End of life care (EOLC): It refers to the health care process that is provided during the last few hours, days or months of life. It encompasses care and support for the patient’s mental and emotional needs, physical comfort, spiritual needs and practical tasks.
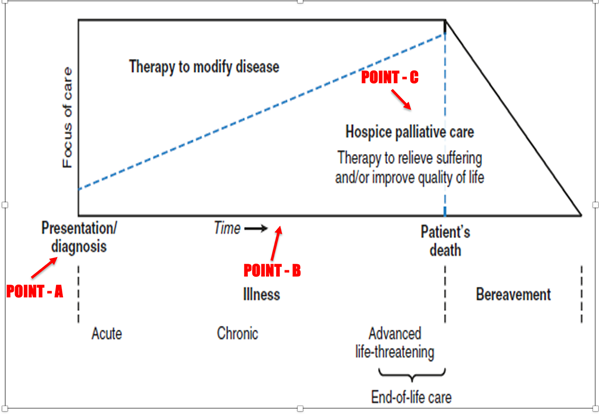
THE GRAPH BELOW SHOWS THE PLACEMENT AND RELEVANCE OF THESE COMMON TERMS DURING THE TRAJECTORY OF CANCER OR A CHRONIC LIFE-LIMITING ILLNESS.
Point A: The period of diagnosis (early palliative care)—when disease-directed therapy is to begin and the counselling is done by palliative care team experts.
Point B: Transition from curative to palliative intent of treatment (timely palliative care)—where the symptom burden, especially in the form of severe pain, psychological difficulties, unanswered questions regarding the future and the need for prognostication, etc., are quite high.
Point C: Transition from palliative intent of treatment towards hospice care or end-of-life care (preparatory palliative care)—where the role of the palliative care team is at its peak. It entails multiple lines of discussion regarding the construction of the current and future care plan, putting the anticipated events into words, planning to complete some unfinished tasks, explaining advanced directives as well as the doctrine of double effect, and preparing for a dignified end-of-life care.
Symptoms Managed By Palliative Care Specialist:
- Pain
- Psychological, spiritual, emotional symptom burden
- Gastrointestinal symptoms like nausea, vomiting, constipation, diarrhoea
- Loss of appetite
- Swelling/Lymphoedema care
- Insomnia and sleeplessness
- Anxiety and depression associated with cancer
- Cough and breathlessness
- Dry mouth
- Infections and wound care
- Ascites/ pleural effusion drainage
Is It Just End Of Life Care?
Palliative care is not just end of life care. End of life care or hospice care is a part of palliative care which is provided during the last few months, days or hours of life.
What Is Respite Care?
While prioritising the patient, carers often end up neglecting their own needs eventually ending up exhausted, drained, frustrated and depressed. Respite care is an integral part of palliative care which is provided when a different person, such as a hospital doctor or nurse, looks after the patient instead of the primary carers so that the primary carers can take a break.